Step 1: Initial Management & Support
- Baby is evaluated and stabilized.
- Nutrition support: high-calorie feeds, MCT oil, and fat-soluble vitamin supplements (A, D, E, K).
- Medications: to improve bile flow and prevent infections (e.g., antibiotics, ursodeoxycholic acid).
Step 2: Kasai Procedure (Hepatoportoenterostomy)
- Timing: Best done before 2–3 months of age.
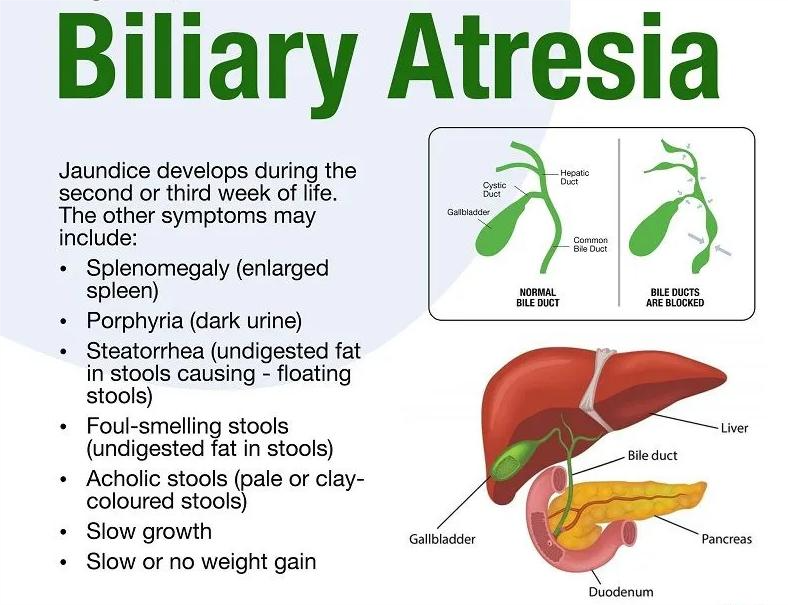
- Procedure: The blocked bile ducts outside the liver are removed, and a loop of the intestine is attached to the liver to drain bile.
- Goal: Restore bile flow, slow down liver damage.
- Outcomes:
- Works well in some babies (especially if done early).
- Others may still develop liver damage over time.
Step 3: Ongoing Care After Kasai
- Regular follow-ups with a liver specialist.
- Continued nutrition and vitamins.
- Watch for complications (cholangitis, cirrhosis, portal hypertension).
- Some children do well for years; others may progress to liver failure.
Step 4: Liver Transplant (If needed)
- If the Kasai fails or the liver is too damaged:
- A liver transplant is performed.
- Can be from a living donor (parent donates part of their liver) or deceased donor.
- Transplant is the only permanent cure for biliary atresia.
- With good follow-up, children can live long, healthy lives after a transplant.